Managing osteoarthritis in dogs and cats
Defining the role of joint replacement in modern orthopedic care.
Canine osteoarthritis (OA) is a progressive degenerative joint disease that transitions from intermittent discomfort to persistent pain as cartilage thins toward bone-on-bone contact. Dogs compensate with altered posture and gait, reduced range of motion, and activity avoidance. Over time, secondary effects include muscle atrophy, weight gain due to lower activity, and behavior changes such as reluctance to play. Overall, OA steadily erodes a dog’s ability to perform normal daily functions and diminishes quality of life for both patient and owner. This article will review surgical management options for terminal OA in the hip, stifle, and elbow joints.
The role of joint replacement
All patients affected by OA benefit from medical management, including activity modulation, professional physical rehabilitation, weight optimization, and medication (including systemic and locally administered drugs). However, because OA is a degenerative process, the success associated with conservative management declines over time. When conservative management reaches its limit, total joint replacement offers a means to remove painful, diseased articular surfaces and reestablish functional biomechanics.
Across all 3 joints, arthroplasty aims to:
- eliminate or substantially reduce pain from bone-on-bone contact;
- restore a more normal range of motion and gait mechanics;
- reduce reliance on long-term systemic analgesics; and
- support a durable return to activity and improved quality of life.
Modern cementless systems rely on osteointegration over approximately 6 to 12 weeks for long-term fixation. This extends the longevity of implants compared with previous implant generations that used cement for fixation. As with any arthroplasty, risks include infection, luxation/instability, and peri-implant fissure or fracture during early healing. Case selection, meticulous soft tissue handling, and structured rehabilitation are central to outcome. Earlier intervention in appropriate candidates typically simplifies surgery and recovery.
Hip joint
Hip OA most often follows hip dysplasia with excessive joint laxity. Abnormal “pistoning” of the femoral head accelerates cartilage wear. As cartilage wear progresses to bone-on-bone contact, pain escalates, and dogs adopt compensations, such as a hip held in relative flexion, avoidance of extension, a tall stance through the tarsus, and abducted resting postures. Additionally, running and jumping become difficult or impossible.
Total hip replacement
Total hip replacement (THR) is a well-established procedure in dogs and has benefited from continuous improvements over the past decades. Historically, THR was reserved for end-stage OA in medium- to large-breed dogs. However, modern implant designs and materials have significantly improved longevity compared with earlier implants, thus supporting earlier interventions. Performing surgery early in life expedites recovery, reduces comorbidities, and minimizes procedural complexity, as the severity of bone stock and soft tissue alterations worsens over time with disease progression. Additionally, product line expansion now enables procedures in small dogs and cats, with expected recovery paralleling that of standard breeds.
Dogs are expected to use their operated leg within 24 hours of surgery, with continuous improvement in comfort levels, quality of life, and function over the following 6 to 12 weeks. The success rate of THR is estimated at 98%, and although serious complications are possible, most of them can be addressed successfully. Complications include luxation, implant-associated infection, aseptic loosening, implant failure, fracture, patellar luxation, neuropraxia, and thromboembolism. Complication rate varies significantly between reports (5%-22%),1-3 but surgery team proficiency and patient selection are considered the most influential factors in mitigating intra- and postoperative complications.
Stifle
Stifle (knee) disease drives most elective orthopedic procedures in dogs, such as tibial plateau leveling osteotomy, lateral suture, and patellar luxation stabilization. Although early outcomes are often rated good to excellent, long-term OA progression varies with chronicity and baseline joint health at the index procedure. Canine total knee replacement (TKR) has been commercially available for nearly 20 years but remains relatively infrequent. Surveys suggest less than 30% are primary procedures, implying many TKR cases are revisions after earlier interventions fail to meet functional goals.
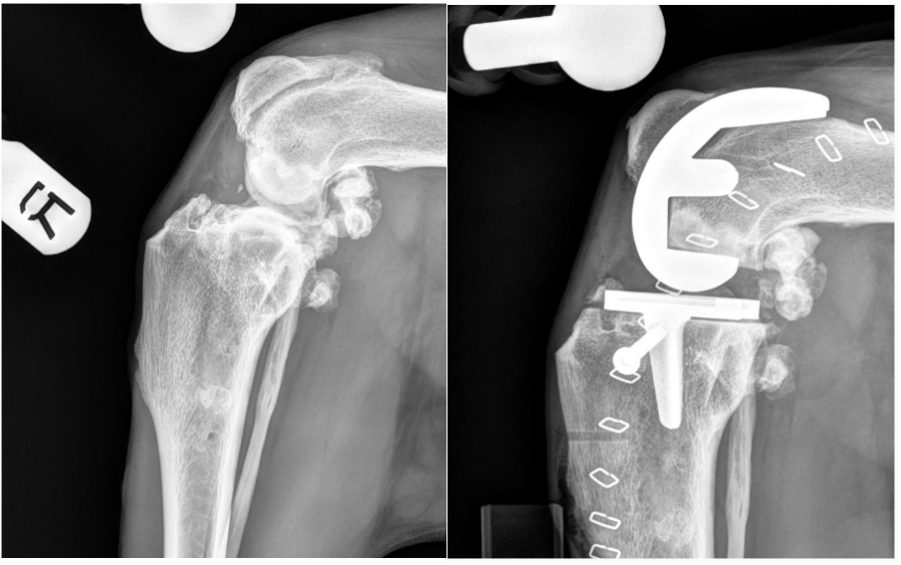
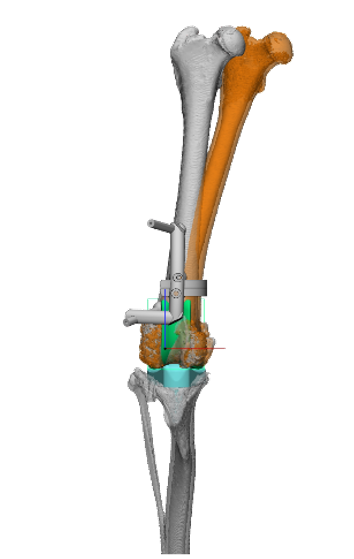
Technique evolution (complication mitigation) changes in surgical approach, along with the development of patient-specific instrumentation (PSI) to improve surgical accuracy, have significantly reduced the risk associated with TKR. In addition, a change in alignment philosophy was made with emphasis on kinematic alignment (KA)—matching implant orientation to the dog’s native alignment and preserving mediolateral soft tissue balance—rather than imposing mechanical neutrality. Early single-institution experience over a consecutive series (approximately 15 cases) reported no collateral failures after adopting the modified approach and KA philosophy.
Outlook
With refined indications, PSI, KA, and robust revision options, primary TKR can outperform standard elective procedures in selected dogs with moderate OA. Wider adoption will depend on formal training and a complete implant ecosystem (including off-the-shelf revision solutions).
Elbow joint
Elbow OA often arises from elbow dysplasia, such as medial coronoid disease or trauma. Progressive cartilage loss produces painful crepitus, swelling, restricted range of motion, and lameness that typically waxes and wanes but trends worse over time, limiting daily function and activity.
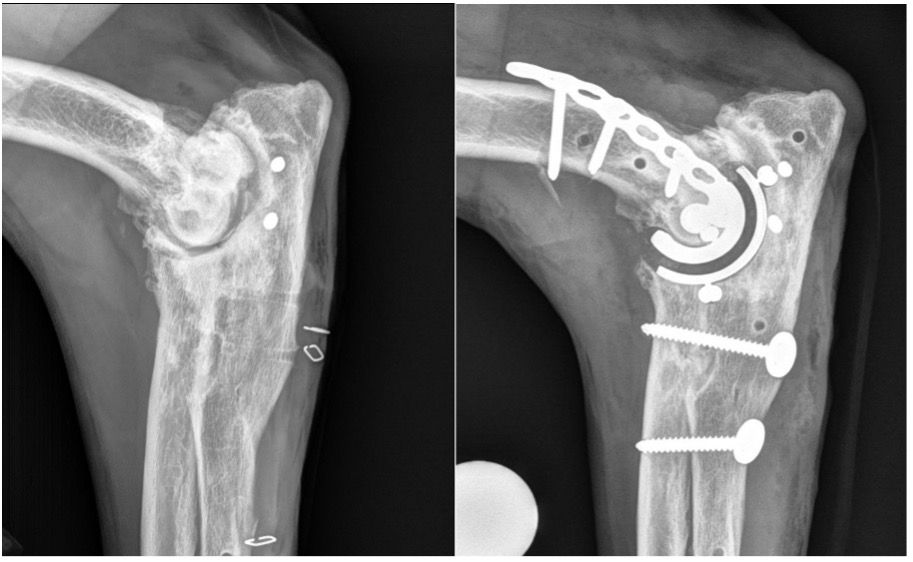
Modern total elbow replacement (TER) uses cementless, porous implants. Current designs couple a humeral component to a radial/ulnar construct with the radius and ulna fused; substantial pain relief is expected, though a residual gait asymmetry is typical due to altered strike mechanics. Many dogs weight-bear early; visible lameness usually improves over 4 to 6 months. Longevity data for current systems are still maturing (earlier generations have shown implant survival for up to 8 years). Key complications include infection (potentially requiring implant removal and arthrodesis), perioperative fissure/fracture, and luxation if collateral integrity is not maintained. Some surgeons employ a lateral approach with PSI to streamline exposure and recovery, recognizing this departs from the original design and requires precise preoperative planning.
Bottom line
- OA consistently reduces canine quality of life through pain and compensatory gait changes.
- When medical therapy plateaus, arthroplasty is the only modality that both removes bone-on-bone pain and restores joint mechanics; durability and expectations vary by joint.
- THR is mature and predictably restores function; TKR is progressing with modern alignment philosophy and PSI; TER provides major pain relief with an anticipated, manageable gait difference and requires diligent follow-up.
- Thoughtful case selection and timely intervention generally improve recovery trajectories and long-term outcomes.
Reference
- Kokkinos P, Parsons K, Belch A, Barthelemy N. The influence of age at total hip replacement on perioperative complications associated with a press-fit cementless stem with lateral bolt in dogs. Vet Surg. 2025;54(3):581-593. doi: 10.1111/vsu.14203
- Kwok JY, Wendelburg KL. Clinical outcomes of canine total hip replacement utilizing a BFX lateral bolt femoral stem: 195 consecutive cases (2013-2019). Vet Surg. 2023;52(1):51-61. doi: 10.1111/vsu.13871
- Allaith S, Tucker LJ, Innes JF, et al. Outcomes and complications reported from a multiuser canine hip replacement registry over a 10-year period. Vet Surg. 2023;52(2):196-208. doi: 10.1111/vsu.13885
- Liska WD, Doyle ND. Canine total knee replacement: surgical technique and one-year outcome. Vet Surg. 2009;38(5):568-582. doi:10.1111/j.1532-950X.2009.00531.x
- Fink BR, Guiot LP, Muir P. Total knee replacement in a dog with an articular epiphyseal medial condylar fracture of the distal femur, a case report. Vet Res Commun. 2025;49(3):142. doi:10.1007/s11259-025-10712-0